Review Article - Journal of Contemporary Medical Education (2023)
Efficacy of a Biophotonics Adjunct in Viral and Microbial Infections
Orien L Tulp* and George P EinsteinOrien L Tulp, Department of Medicine, University of Science Arts and Technology, Montserrat, USA, Email: o.tulp@usat.edu
Received: 20-Nov-2023, Manuscript No. JCMEDU-23-120572; Editor assigned: 24-Nov-2023, Pre QC No. JCMEDU-23-120572 (PQ); Reviewed: 08-Dec-2023, QC No. JCMEDU-23-120572; Revised: 15-Dec-2023, Manuscript No. JCMEDU-23-120572 (R); Published: 22-Dec-2023
Abstract
Discovery and development of effective strategies to treat emerging and often drug resistant strains of viral and microbial pathogens presents one of the greatest challenges of the 21st century. Despite nearly a century of progress in developments in antimicrobial and antiviral therapies, infectious diseases still account for a substantial proportion of deaths worldwide. This toll includes over 100 million globally in the recent pandemic to date. In recent decades, the plague of antimicrobial resistance has also represented an additional and alarming signal for both human and animal healthcare and now signals a renewed sense of urgency in addressing this issue. This has made the search for novel classes of antibiotics, antivirals and therapeutics found to be capable of bypassing the microbial and viral resistance mechanisms necessary. Thus, attempts to replenish our current arsenal of antimicrobial and antiviral drugs and update our therapeutic regimens remains a key priority. In addition, the tremendous impact exerted by viral infections and related pathologies on our lives during the recent decade has forced scientists to acknowledge the opportunities and challenges associated with tackling infectious diseases. This challenge can only be met by developing effective antiviral agents that may be endowed with novel mechanisms of action. The discovery of new antimicrobial/antiviral agents, as well as the repurposing of existing drugs and therapeutic options will be crucial to fight the ever-increasing resistance of “superbugs”, pathogenic fungi, viruses, and parasites. Some proponents of modern biophoton therapy discussed in this paper can trace their origins to the Russian scientist Alexander Gurwitsch. A century ago, Gurwitsch observed ultra-weak emissions of light emerging from an onion root, and soon found additional living tissues to be emanating similar energetic phenomena. Thus, Gurwitsch’s energizing research which continues to the present day was projected toward the development of useful applications of the new-found biological photonic phenomena. The purpose of the present paper is to introduce the past experiences with forms of biophotonic therapy. This includes potential applications and some highly successful outcomes of biophotonic therapy when used as an option to treat infectious diseases including HIV, Hepatitis C, MRSA, and others. These observations included an emphasis on efficacy of using biophotonic therapies to treat and ameliorate the drug resistant variants of the above infectious agents. The discussion includes potential applications for the current COVID-19 pandemic and in addition to preparation for the emergence of the next epidemic or pandemic.
Keywords
Epidemics; Pandemics; Severe Acute Respiratory Syndrome (SARS); Covid-19; HIV; MRSA; Biophotonics adjunct; Energy dynamics; Electromagnetic therapy; Irradiation; Immunomodulation; Infectious illnesses; Drug resistance; Therapeutic efficacy
Introduction
Discovery and development of effective strategies to treat emerging and often drug resistant strains of viral and microbial pathogens presents one of the greatest challenges of the 21st century. Despite nearly a century of progress in developments in infectious disease therapies, they still account for a substantial proportion of deaths worldwide including over 100 million globally in the recent pandemic. In recent decades, the plague of antimicrobial resistance has also represented an additional alarming signal for both human and animal healthcare and now signals a renewed sense of urgency in addressing this issue. This has made the search for novel classes of antibiotics, antivirals and therapeutics found to be capable of bypassing the microbial and viral resistance mechanismsnecessary. Thus, attempts to replenish our current arsenal of antimicrobial and antiviral drugs and update our therapeutic regimens remains a key priority in global healthcare. Additionally, the tremendous impact exerted by viral infections and related pathologies on human lives during the recent decade has forced scientists to acknowledge the opportunities and challenges associated with tackling infectious diseases. This challenge can only be met by developing new, effective agents that may be endowed with novel mechanisms of action.
The discovery of new antimicrobial/antiviral agents, as well as the repurposing of existing drugs and therapeutic options will be crucial to fight the ever-increasing resistance of “superbugs”, pathogenic fungi, viruses, and parasites. Some proponents of modern biophoton therapy can trace their origins to the Russian scientist Alexander Gurwitsch, who a century ago observed ultra-weak emissions of light emerging from an onion root and soon found additional living tissues to be emanating similar energetic phenomena. Thus, Gurwitsch’s energizing research was projected toward the development of useful applications of the new-found biological photonic phenomena. The purpose of the present paper is to review historical experiences with biophotonic therapy when used as an adjunct to treat numerous infectious diseases including HIV, Hepatitis-C, MRSA, and others, including treatment of drug resistant variants of the above agents and the proposed adoption of biophotonics in addressing the next epidemic or pandemic. Many agents of what we now recognize as agents and vectors of communicable infectious diseases include some that have plagued mankind since the beginning of recorded history. Communicable infectious illnesses have often resulted in epidemics that were sometimes followed by pandemics, and in the unfortunate deaths of many who were to become afflicted with the infectious agents of those eras [1]. The gradual progression of humankind from residing in ethnically and culturally remote locations from each other has now merged into larger and more condensed residential communities. As regional population densities increase, the potential for person-to-person transmission of infectious agents also becomes increased. These progressive changes in population dynamics may bring about the epidemiologic potential to infect many unsuspecting and immunologically unprepared individuals in a shorter duration of time. The discovery and scientific identification of many of the causative organisms led to the subsequent development of public health measures and protective vaccines. In addition, the vaccines when coupled with antimicrobial and antiviral agents have saved countless lives during the past century. However, in the real world, many of the infectious agents soon express internal survival mechanisms which enable them to adapt to the presence of chemically mediated antimicrobial and antiviral actions. The expression and development of chemical resistance mechanisms essentially neutralizes the impact of the chemical agents, and thereby enables the invasive agents to continue to flourish in their hosts. These microbial and viral survival attributes have created a pressing need to develop newer and more effective therapies to more effectively control their often aggressive and deleterious spread [2].
The discovery and redevelopment of photonics during the last century marked a new era in the development of non-chemical strategies to treat and control the spread of infectious illnesses of man and animals [3]. These redevelopments resulted in life-saving impacts where antimicrobial therapies alone proved unsuccessful [3,4]. A brief history of infectious diseases in societies over the ages, and proposed molecular mechanisms and clinical applications of biophotonic therapy to treat drug resistant strains of HIV, Hepatitis C, MRSA and other infectious agents yet to emerge and impact society are summarized [4]. The recently emerged coronavirus strain that caused COVID-19 illness is the newest member of the Coronaviridiae family to emerge. This strain is well known to produce respiratory, gastrointestinal and other illnesses in man and animals [4-7]. Although the exact source or origin of the SARS-COV-2 virus remains unconfirmed, coronavirus strains have been isolated from other mammalian species but have been found to cause less severe respiratory and other illnesses in humans [6-8]. Thus, while the human infections could have passed from an intermediate animal host via incidental interspecies transmission of other epidemiological sources as it has for MERS, its origins remain unconfirmed, and evidence of interspecies transmission for COVID-19 remains speculative [9].
The SARS 2-COV-19 virus emerged in Wuhan, China in 2019, has subsequently spread exponentially worldwide during the Spring to Fall of 2020 and had infected millions of people globally by late 2020, with some resulting in death or other dire chronic consequences. Since the first report numerous new infectious COVID-19 spike mutations have evolved, some with an even more highly infectious potential than that of the initial virus. Infections globally stand at approximately 700 million to date; continuing outbreaks of viral mutants have continued to emerge, often evading immunities formed from vaccinations and ‘natural immunity’ from earlier variants of the virus [9-13]. Prior to the introduction of antimicrobial and antiviral agents during the mid-20th century, the process of biophotonics had often been employed in various forms as a method to combat the progression of infectious illnesses [3,4]. The use continued until being replaced by the newer, conventional pharmacologically based therapies, which have contributed to the successful treatment and of millions of lives saved from infectious illnesses to date [14]. Over time however, many infectious organisms may continue to not only survive but to thrive in their hosts with seeming impunity. When the infectious agents successfully reemerge by developing resistance mechanisms to overcome sensitivity to the chemical agents, they now pose an additional threat to host survival.
Biophotonic treatments had been utilized successfully to treat infectious illnesses worldwide for decades prior to the development and adoption of pharmaceutic agents [3,4]. Pharmacotherapy remains the current standard of care in present-day therapies for most infectious diseases [14]. In contrast, reports of microbial and viral resistance have not been observed following biophotonic therapy. Thus, biophotonics may re-emerge as a safer long-term alternative and may be able to facilitate the eradication of infections without significant side effect. The proposed applications include but are not limited to the coronaviridiae, HIV, MRSA, and other active infectious illnesses of interest. Because reports of the development of microbial or viral resistance to biophotonic therapies are nil, it may have virtually unlimited use in infection control in the future. Previous reports indicate that the apparent eradication or amelioration of the infectious agents via biophotonic treatments have been complete. Beginning some 10,000 years ago the evolution of urbanization of more closely connected communities began and has provided infectious diseases with greater opportunity to merge into larger clusters of illness, and to progress as epidemics and pandemics [1]. With the advancement of global travel opportunities in recent centuries, epidemics now have an additional opportunity to travel abroad with their infected hosts, thereby opening the floodgates to enable their expansion and progression into epidemics and pandemics. Diseases like influenza, smallpox, leprosy, malaria, tuberculosis, and others are identified among those that have thrived virtually worldwide since this shift in population demographics, infecting unsuspecting and unprotected individuals on every continent except Antartica [1]. As human civilization has evolved and communities have become better connected, the likelihood of epidemics progressing to pandemics have also become better connected. Thus, the infectious agents of old have subsequently continued to evolve, propagate, and plague new hosts to the present day. Advances in sanitation and in the discovery and development of efficacious, cost effective, and potentially curative antimicrobial and antiviral pharmacotherapeutics over the past century have become the best but not the only defense [15,16].
Examination of the history of infectious diseases causing epidemics and pandemics over the past 2500 years suggests they will likely continue to affect our modern-day lives. Pandemics can strike with a vengeful force, often leaving few survivors in their wake. The emergence of epidemics and pandemics dictate a need for efficient, effective, and cost-effective mechanisms to deflect their impact on health and survival not only for the ‘fittest’ but for all peoples left in their swath of infectious influence; pharmacotherapeutics alone are not likely to be the only solution. Proponents of modern biophoton therapy can trace its origins to the early discoveries of Alexander Gurwitsch and his observations of ultra-weak light emissions from preparations of onion roots and living tissues, indicative of a bioenergetics phenomenon [3]. These observations energized momentum to further identify and develop useful applications of his newfound scientific finding, now recognized as the birth of biophotonics.
Historically, epidemics and pandemics have occurred intermittently for nearly 2500 years and have changed the course of history from their earliest known occurrences. Infectious agents are immune from any specific population group, and can infect individuals of all social, political, religious, economic, or cultural identity equally, often with dire consequences [1]. As the early civilizations expanded into larger populations and empires, their leaders conquered different and more distant parts of the world, which enabled prevalent infectious diseases then of unknown origin to gain more opportunities to spread to the new destinations. In return some of the conquered populations also graciously helped to unwittingly spread their infectious agents to their conquerors and new-found hosts. These ancient exchanges of infectious diseases are also credited with the first known instance of biowarfare using an infectious agent.
Literature Review
History of epidemics and pandemics
The first recorded incident of an early form of biowarfare occurred during the siege of Athens, Greece during the Peloponnesian War (430 B.C.), where the conquers thrust the infectious agent over the Athenian walls [1]. The ensuing plague resulted in a pandemic that claimed approximately two thirds of the Grecian population and led their conquerors to victory. Some 600 years later, the Antonine plague of 163 A.D. is now believed to have been an early strain of smallpox that began with the Huns, who then passed the infection to the Germans and Romans, who then transported it throughout the expanding Roman empire, causing millions of deaths throughout the empire. The Cyprian plague epidemic broke originated in Ethiopia around 250 to 550 A.D. and spread throughout Northern Africa and as far North as Rome, resulting in millions of deaths along the way. The Justinian plague broke out in Egypt in 541 A.D. and quickly spread across nearby Palestine and the Byzantine Empire, finally reaching the Mediterranean, and ultimately resulted in the deaths of over one quarter of the known world populations of the time. This illness is now suspected to have been an early entry of the first significant emergence of the bubonic also called the ‘Black’ plague, caused by Yersinia pestis (Y. pestis; formerly Pasteurella pestis). The infamous Black plague pandemic lasted for several centuries is believed to have occurred in Europe. The prevalence of subsequent epidemics began during the siege of the Genoese trading port of Kaffa in Crimea by the Golden Horde army of Jani Beg in 1347, where it likely originated previously [1]. Once established in Crimea, the infectious agent was most likely transmitted by fleas from rats that typically travelled on trading Ships, which enabled it to spread throughout the Mediterranean Basin. From seaports, it gained entry to the surrounding lands of North Africa, Western Asia, and Europe over the next five centuries. The bubonic plague made another grand entrance of major proportions in 14th century Europe, where it is generally believed to have resulted in the deaths of over half of the European population. The bubonic plague re-emerged again in England in 1665 where it was known as the ‘Great Plague of London,’ and resulted in the deaths of 20% of the city’s population during its deadly reign. The bubonic plague has now resulted in the deaths of over 100 million people, and annually the World Health Organization currently reports between 1000 and 2000 cases of the bubonic plague. The bubonic plague occurs most commonly in Madagascar and Sub-Saharan Africa, where it continues to spread via flea infested rodents and person to person contact.
Recent genomic analysis of specimens obtained from ancient skeletal remains have now been linked to the various strains of Y. pestis that were causative of the numerous epidemics throughout the world. The genomic analysis has provided confirmation of the origins and continuity of the bacterium over the many centuries of its known existence [17]. Leprosy, now known to be caused by the bacteria Mycobacterium leprae had its origins during the 11th century A.D. and became prevalent in Europe. Although the infection is now highly treatable with antimicrobial agents, it still occurs in sporadic instances in numerous countries where it spreads by person-to-person contact. Prior to the development of chemical agents to treat infectious disorders, most indigenous residents applied various concoctions of natural products in attempts to ameliorate the symptoms of their illness. Thus, the early therapeutic approaches with natural products in ancient times established the groundwork for the fields of natural medicine and modern-day pharmacotherapeutics as we know them today [15,16].
Measles, a highly contagious illness caused by a strain of the Rubeola virus spreads via droplet infection and can cause severe illness in naïve and unvaccinated populations. As early as 1875, the Pacific Island nation of Fiji suffered an epidemic of measles virus during which approximately one third of the Island population were infected, and between 40,000 to 120,000 individuals died because of the complications from the measles virus. The high rate of infectivity may occur during the early manifestations of illness during the first week of host incubation, before symptoms become prominent, and prior to the clinical appearance of the typically diagnostic rash and secondary symptoms. Highly effective measles vaccines were developed more than a half century ago, and in recent decades, availability of the vaccines has prevented most of the new measles related illness to occur by initiating the vaccination process during the first year of life. During early life, infants and young children can fall subject to the most severe symptoms of the illness, and despite global vaccination programs that now reach over 90% of the population in most countries, clusters of the illness still occur mostly in unvaccinated individuals. The WHO has reported that in 2018 measles infections still claimed the lives of over 140,000 people, mostly in unvaccinated children under the age of 5 years who died because of respiratory and other potentially severe complications of Rubeola virus infection [1].
Cholera epidemics caused by toxigenic strains of the Vibrio cholerae bacterium have also occurred for centuries. The infection is usually spread via the fecal-oral route through contaminated water sources, which commonly occur following environmental disasters [18-20]. The V. cholerae bacteriumis a diverse microbial species of over 200 strains and includes both pathogenic and non-pathogenic variants [18,19]. Only the toxigenic or toxin-producing serologic V. cholerae-01 and V. cholerae-0139 strains are associated with cholera epidemics, however. Cholera illness causes severe acute symptoms including watery diarrhea, dehydration, and loss of electrolytes within the first 2 days of the infection, and if left untreated, can be life-threatening or fatal within hours or as little as 2 to 3 days after infection, even in previously healthy people [19]. Cholera represents another common cause of epidemics which continues to be a threat to the present decade. The infection is noted for the classic ‘4 Ds’ often associated with the illness: Diarrhea, dehydration disorientation and death. Cholera outbreaks often occur following environmental disasters that disrupt the consumable water supplies of affected regions. Since the first major outbreak of Asiatic cholera in Calcutta in 1817 there have now been seven cholera epidemics of significance during the past two centuries, including reports of cholera outbreaks in the Asia, and the cities of Muscat, Tehran, Baghdad, Port au Prince, Haiti, and others [1].
Haiti had been considered Cholera-free with no cases reported for at least 100 years. In 2010 however, an epidemic occurred following a massive earthquake in Port-au-Prince on January 12, 2010, which caused massive damage to community water sources and caused one of the worst cholera outbreaks in modern history [18]. The Haiti epidemic is thought to have been caused via imported aid workers who disposed their contaminated refuse into the community river. The epidemic resulted in approximately 820,00 cases and nearly 10,000 fatalities during the ensuing decade, and a brief resurgence in 2022 resulted in over 600 additional confirmed cases [20]. The majority of the cases occurred in the greater Port-au-Prince area, the major location of the 2010 earthquake damage, much of which is still awaiting recovery although the major water sources are now deemed safe [18].
Despite improvement in water quality and safety measures in many counties, cholera outbreaks still remain an epidemiologic threat. Because cholera illness encompasses a broad spectrum of symptoms, especially in endemic areas where many affected individuals may become acclimated to harboring a chronic infection and developing a partial immunity and may become carriers and continue to spread the infection to others. Active cases that receive effective treatment likely remain vastly underreported, as are precise measurements of the morbidity and mortality attributable to V. cholerae infection are incomplete. Despite public education and improvements in the quality and safety of potable water supplies there are still an estimated 3 to 4 million cases of diarrheal illness and approximately 100,000 fatalities worldwide annually, caused by toxigenic strains of V. cholera [19]. Cholera remains endemic in approximately 50 counties, including Africa, Asia, the Middle East, Mexico, South and Central America, and the Caribbean. The infection may occur wherever there is inadequate access to clean water and sanitation, where it can cause serious illness in unsuspecting, naïve and nonimmunized visitors to those countries.
Seasonal Influenza remains a serious threat, despite an abundance of flu vaccination programs. The first of the influenza pandemics materialized with the Russian flu pandemic of 1889, where approximately 360,000 people died from influenza infection [1,21]. The far more deadly Spanish flu pandemic caused by the H1N1 influenza strain emerged in 1918, costing the lives of over 50 million people across the globe before it subsided. It was followed by the more recent Asian flu pandemic which persisted for several years during the mid-20th century. Nearly forgotten was the so-called ‘Swine Flu’ scare of the mid 1970s, where a strain of influenza with an immunologic footprint that was similar to the 1918 flu emerged briefly, but the timely implementation of widespread immunization to the most susceptible sectors of the US population was deemed a factor in preventing further outbreaks of the illness [21]. The third influenza pandemic arrived in 2009, also designated the ‘Swine flu’ was a variant of the H1N1v strain and persisted through 2010. The recent H1N1v and related variants resulted in over 300 hospitalizations but very few deaths were reported. The H1N1 Swine flu was so named because it is a virus that primarily infects swine, and variants (designated with a ’v’) exhibit only limited transmissibility to humans and result in a milder disease and illness than were caused by the 1918 strain.
Another minor influenza virus with respect to human infection is the Avian flu, designated as Asian HPAI/H5N1 or LPAI/H5N1 virus, common to domestic poultry and endemic in certain countries of the world including Bangladesh, China, Egypt, India, Indonesia, and Vietnam according to The United Nations Food and Agriculture Organization data [21]. The virus has now spread to many additional countries, in part via seasonal migration of infected birds. In January 2015, the HPAI H5N1 virus detected in a wild duck in the United States was found to be a “reassortant” virus that contained genes from Asian HPAI H5 viruses and Low Pathogenic (LP) North American viruses. The January 2015 reassortment virus is not known to have spread indiscriminately since its discovery.
The genetic process of viral genetic “reassortment” occurs when the genes from two or more different viruses blend together to create a new virus as appears to have occurred with the recent SARS-N-CoV-19/COVID-19 virus. During the process the newly formed virus substrain may either gain or lose some properties, as appears to have occurred with newly emerging mutated strains of the COVID-19 virus [22,23]. The HPAI H5N1 virus detected in the United States was a new combination of Avian influenza genes never previously discovered. While no human cases associated with this reassortment virus have been reported, it remains possible that this virus could infect people and cause serious disease in the future. Accordingly, the CDC has developed interim guidance on testing and prophylaxis procedures for the Avian flu virus. To date, fewer than 1000 nonfatal cases having been reported worldwide. However, it would seem prudent to review the CDC-developed interim guidance on Avian flu testing, prophylaxis and clinical guidelines as a precaution [21]. The final pandemic of the 20th century was the Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (the HIV or AIDS virus), discovered in 1981 and still flourishing throughout the world [1]. HIV/AIDS is generally considered to be a sexually transmitted illness of humans, as the most common form of its transmission is person-to-person contact often following unprotected sexual activity or use of contaminated needles. Infection with the HIV/AIDS virus has now been attributed to over 30 million lives lost to date. The virus progresses slowly once an individual is infected, often taking months or years to become fully clinically manifest, and during the prolonged incubation, unsuspecting carriers can easily transmit the infection to additional individuals. Thus, the usual slow progression of the HIV/AIDS illness has enabled this pandemic to continue for a much longer duration and yield more dire consequences than occurs with most typical infectious agents. Because the clinical manifestations of HIV infection progress more slowly than most other infectious diseases, infected individuals may remain unaware of their infection for weeks to years before any suspicions of illness appear. Four decades of scientific research and discovery has led to several pharmacologic agents that ultimately may slow the progression of the virus and prolong the survival of the infected individual, but sadly, a definitive cure is still in the future. Accordingly, the final outcome is often dire regardless of the duration of the illness and even in the face of antiviral drugs that may only slow the progression; the impending death of the individual remains the anticipated final outcome. The spread of HIV/AIDS is still considered to be an active pandemic, as more than 32 million lives have been lost worldwide to this disease over the past four decades [1].
The COVID-19 pandemic is the first reported pandemic of the 21st century and became prevalent throughout most of the world during 2020 and 2021. In the current decade, the onset of the COVID-19 outbreak was first reported to the WHO from Wuhan, China in late December 2019 and soon spread through much of the globe due to the ease of international travel, causing panic and apprehension among all in its fateful path [6-12]. The pandemic left few effective options for easy containment due to its efficient airborne microdroplet mode of transmission. In addition, no clear treatment or containment protocols or pharmacotherapeutic agents had been established in part due to a paucity of information as to the pathophysiologic nature of the virus and the broad diversity in patient symptomologies [10]. Prior to 2020, little was known about the new strain of virus other than it was more highly contagious and caused a more serious respiratory illness than the previously known related strains that had caused MERS and SARS [10-12].
The WHO declared COVID-19 to be a pandemic in early 2020 and by late February 2023, the number of COVID-19 cases reported worldwide had reached almost 680 million and the number of deaths reported exceeding 6 million individuals [13]. Those most severely impacted were individuals with comorbidities including obesity, diabetes, cardiovascular and respiratory disorders, compromised immunocompetency and over the age of 65 [24-26]. The complete numbers of patients confirmed to have become infected or died from the virus may never be known due to presumed incomplete reporting and inadequate availability of reliable diagnostic criterion. Those issues, in concert with strained economic and medical resources by some countries have contributed to the uncertainty of its impact on global health and longevity. Also, the recognition of prolonged symptoms, now designated as a ‘long COVID’ syndrome add to the complexity and aftermath of the pandemic [12,26-28]. Multiple vaccines and boosters were developed and marketed in less than a year from the outset of their development, marking this the shortest time to develop, test and release a new vaccine in history in any nation, but have failed to fully prevent infections [11].
Limitations of pharmacotherapy
The development of microbial and viral resistance often poses virtually insurmountable barriers to effective treatment and may be overcome via biophotonic therapies. The development of viral and antimicrobial resistance to conventional therapies enables infectious diseases to continue to be among the most significant causes of morbidity and mortality worldwide [1]. Globally, they are often associated with a lack of appropriate environmental or institutional availability of adequate diagnostic and effective treatment options [2,3]. The impact of drug resistant infectious diseases on health and well-being may occur independently of the relative affluence of a population or other epidemiologic factors of the affected community and may result in dire outcomes especially where vigorous antimicrobial and antiviral resistance of the invasive agent has intervened [4]. Because infectious organisms often express an innate epigenetic ability to neutralize the effects of administered chemical agents that could otherwise spell their premature demise, especially when the treatment regimen has been unsuccessful, alternative therapies are deemed essential. The host capacity for immunocompetence and immune protection also normally plays a supportive role to pharmacotherapeutics delivered by chemical agents. The host immunocompetence may easily become overcome in the absence of adjunctive treatment factors when exposed to resistant strains of an infectious agent.
Scientific research of RNA coronaviruses impacting the current pandemic has been developing for over two decades and continues to be of extreme necessity, considering the recent pandemic [9-11]. These research studies culminated in numerous clinical trials of multiple newly developed COVID-19 vaccines in 2020, which applied the recently developed mRNA and other molecular models, and with recommendations for booster shots that encompassed recently evolved epitopes discovered later in some of the more prevalent mutant sub-strains as the pandemic continues to evolve. Episodes of COVID-19 infections and reinfections are also reported to occur commonly in individuals who had been vaccinated with the newly developed vaccines in addition to others who had developed natural immunity by contracting the virus prior to or after vaccination due to an apparent transient nature of the immediate immune responses following vaccination or infection [6-10]. The immunogenic spike protein mutations appear to bypass earlier immune protections especially those with significant comorbidities [9,10,24-28]. Those deemed at greater risk typically require additional emphasis for early treatment in an attempt to limit post infection sequelae including the development of long COVID symptoms, which may develop in 5% to 15% of those infected and persist for a year or more [9-12,28]. Autoimmune and related diseases may complicate treatment strategies, and the range of symptoms often overlap in patients with chronic autoimmune diseases, obesity, and other common comorbidities because the pathophysiologic mechanisms associated with COVID-19 illness and other comorbidities may differ [26]. Thus, it becomes important to discriminate among the possible therapeutic regimens that may be prescribed for COVID-19 and other overlapping conditions to best effect the success of the therapeutic regimen for each concurrent disease entity.
Biophotonics therapy is not known to result in harmful side effects and is of interest because of the many deaths reported worldwide may have been preventable had biophotonics treatment been applied in a timely basis. Additionally, in many individuals, the coexistence of COVID-19 and one or more comorbidities likely added additional complications, and the virus may have been incidental to the patient’s demise. When present, comorbidities may complicate or cloud a more accurate or precise diagnosis in the absence of virus-specific serologic analysis [14]. Among those who have tragically succumbed, some cited COVID-19 as the direct primary cause, while for many others, the pathophysiologic sequela of COVID-19 including increases in plasma availability of inflammatory cytokines was additive to a pre-existing comorbidities as contributing factors to the patient’s demise [11-14].
The present Review is based on retrospective analysis and review of patient outcomes using biophotonic therapies as a primary treatment regimen for patients with confirmed HIV and MRSA, but may be applied to other infectious illnesses as well [4]. The infectious illnesses were treated with biophotonic therapy outlined in the Einstein Matrix protocol in the Einstein Medical Laboratories Clinic in the Dominican Republic since year 2000 [4,29,30]. While no specific reports of biophotonics treatment for COVID-19 have emerged to date, the broad spectrum of antimicrobial and antiviral effects of the UV radiation strongly suggest that it would be equally as effective as it has proven for other infectious illnesses. The molecular mechanisms of UV irradiation and biophotonics treatments are well known;multiple events connected to UV irradiation may induce both beneficial or damaging effects on tissue viability, depending on the wavelengths encountered, the intensity and duration of the UV exposure, and the tissues exposed in vivo or as an extracorporeal quasi–in vitro exposure typically produced in freshly obtained whole blood.
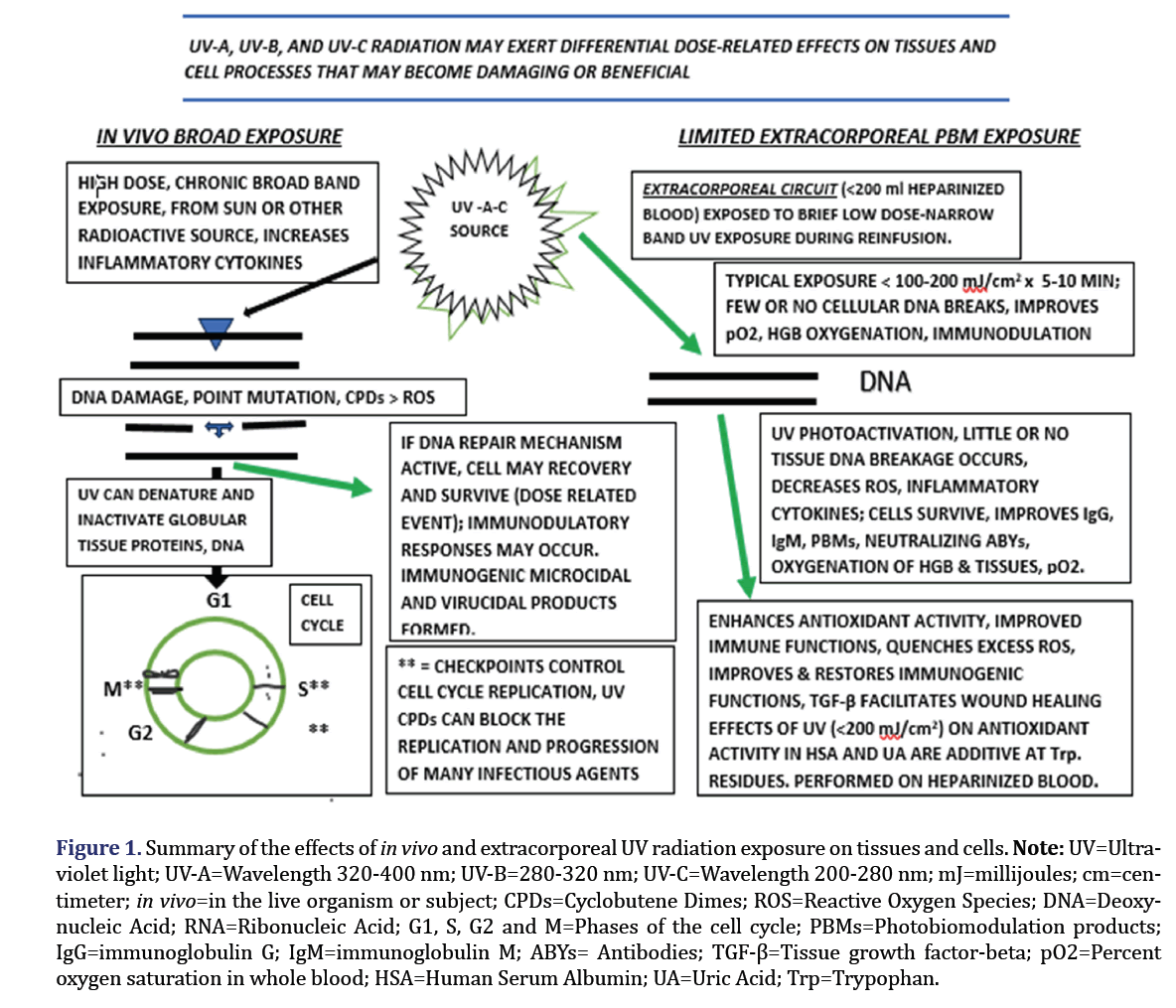
A summary of the effects of UV and the biophotonic and biophotomodulatory actions on cells, tissues and infectious agents is depicted in Figure 1 below. The potentially damaging effects of extreme exposure as may be caused by excess solar exposure are summarized on the left side of the diagram, and the effects of extracorporeal biophotonic exposure depicted on the right side of the figure. In biophotonics therapy depicted on the right side, an aliquot of the patient’s whole blood is typically diluted in sterile, normal saline and re-infused immediately after controlled low dose UV exposure, and within 30 minutes of its initial removal from the subject (Figure 1). Thus, the contributory biochemical mechanisms resulting from low-vs. high-dose biophotonic exposure to infectious agents differ markedly from the established mechanisms of microcidal and virucidal action that occur for traditional pharmacotherapeutic agents. On the left side of Figure 1, biophotonic UV irradiation treatment conducted over a broad range of the ultraviolet spectrum has the capacity to disrupt and denature viral and microbial nucleic acid protein structures respectively, thereby initiating virucidal and microcidal actions. The virucidal and microcidal actions damage genomic mechanisms and induce post-exposure prevention of their authentic in vivo replication processes in the host [4,30,31].
Figure 1: Summary of the effects of in vivo and extracorporeal UV radiation exposure on tissues and cells. Note: UV=Ultraviolet light; UV-A=Wavelength 320-400 nm; UV-B=280-320 nm; UV-C=Wavelength 200-280 nm; mJ=millijoules; cm=centimeter; in vivo=in the live organism or subject; CPDs=Cyclobutene Dimes; ROS=Reactive Oxygen Species; DNA=Deoxynucleic Acid; RNA=Ribonucleic Acid; G1, S, G2 and M=Phases of the cell cycle; PBMs=Photobiomodulation products; IgG=immunoglobulin G; IgM=immunoglobulin M; ABYs= Antibodies; TGF-β=Tissue growth factor-beta; pO2=Percent oxygen saturation in whole blood; HSA=Human Serum Albumin; UA=Uric Acid; Trp=Trypophan.
The quanta of photons derived from light are deemed a prerequisite for health, and as such, humans have always instinctively sought daylight and sunlight as nature’s natural cure-all for many sorts of illnesses including infectious illnesses and wound healing [3]. The oldest reference for sunlight UV light irradiation for infectious illnesses of humankind dates to on or before 1500 B.C [1-3]. Although the molecular mechanisms of these light-derived effects have long remained unknown, unconfirmed, or speculative at best, emerging findings now point to a nuclear disruptive element which impedes further replication of the infectious agent, combined with enhancement of immune responses in the UV-exposed host. The process of photobiology requires the presence of a specific photo acceptor molecule or complex, which after photonic excitation could induce the downstream activation of signaling pathways to bring about its desired healthful or other responses. Both ionizing and non-ionizing radiation can cause mutations in DNA of cells, albeit through different molecular mechanisms. Strong ionizing radiation such as high-energy UV-C, X-rays and gamma irradiation can produce both single- and double-strand breaks in the nucleotide and nucleoside backbones through the formation of hydroxyl radicals and other biochemic events. In contrast, exposure to non-ionizing radiation can induce the formation of dimers between two adjacent pyrimidine bases of RNA. In both cases of ionizing or nonionizing exposure the usual consequence is the denaturation of the viral genome which prevents further replication of the infectious agent. Rather than denaturing or damage to the protein and lipid envelopes, genomic damage is likely to be the primary target for irradiation-induced viral inactivation [24-28].
The effectiveness of UV radiation as a disinfectant however is now known to be dependent on the wavelength range of the incident photons to which a tissues have been exposed [21-33]. The three primary UV bands are: UVA (320-400 nm), UVB (280-320 nm), and UVC (200-280 nm), with UVC containing the strongest UV light with the most potent antiviral and antimicrobial properties. The UVA band is less energetic but up to 20 times more intense than that of UVB or UVC. The UVC band can induce the formation of Cyclobutene Pyrimidine Dimers (CPDs) in addition to a variety of oxidatively generated lesions, including single strand RNA breaks and oxidized bases that effectively impede further host replication of the viral or microbial genome. Exposure to the UVB band can also lead to the formation of CPDs and other damaged photoproducts including pyrimidine (64) pyrimidones (64PPs). The 64PPs are also inhibitory to in vivo genome replication in host tissues. Finally, exposure to the UVC band also causes photochemical structural damage to both DNA and RNA polymers. UVC can disrupt cross-linking events and generate oxidative damage to the nucleotide bases which prevents further genomic replication of the infectious agent. Follow up phototherapy with red light (wavelength of 660 nm) may further enhance the biophotonic responses as red light irradiation enables the participating entities to absorb energy, which can then be transferred to viral oxygen molecules. The increased oxygenation processes result in making the genomic residues more highly oxidized and cause further irreversible damage to the membranes and genomic material of several viruses, including hepatitis C, HIV and others [30-33].
Thus, from the above discussion, all UV irradiation bands can deliver immunogenic microcidal and virucidal products. The immunogenic products can then generate immunogenic actions from the immune-stimulating byproducts of the UV irradiation, and the immune-stimulating byproducts can now stimulate and enhance immunological events in an immune-responsive host organism. In the case of DNA viruses, two major UV-induced lesions, pyrimidine CPD dimers and 64PPs both arise at the same nucleotide sites, are both lethal and mutagenic. In contrast, the presence of uracil vs thymine nucleotides in RNA gives rise to the formation of several RNA photoproducts, including uracil dimers that can inhibit reverse transcriptase activity, thereby preventing further host replication and the generation of new virions. The propagation mechanism of SARS-CoV-2 of the current pandemic is independent of reverse RNA transcription and genome integration that occurs in non-encapsulated viruses. However, the UV-induced RNA lesions can still lead to the formation of uracil dimers, capsid instability and degradation, and covalent binding of proteins to the viral RNA. These effects can then contribute to the immunogenic host responses. Imposing UVC irradiation also causes oxidative damage to viral capsid proteins in non-enveloped viruses, further contributing to UV-mediated virucidal actions.
The conventional UV lamps used in biophotonic therapies often use mercury discharge and low-pressure mercury vapor lamps with a strong emission peak at 254 nm. which is close to the RNA absorption maximum at 260 nm and within the therapeutic range that can deliver virucidal and microtidal actions. In contrast, UV LEDs when used as an alternative source of irradiation are not only environmentally safer than mercury sourced emission lamps but are also more compact, more energy efficient, lower-cost and longer-lasting and will likely replace the older technologies in the future [29-32]. As reviewed above, the delivery of incident photons from UV sources of irridiation via photobiomodulation can cause structural damage to proteins and genomes of infectious agents, and in so doing, can generate denatured entities that can now stimulate the host immune system as foreign, unrecognized proteins. Foreign proteins can stimulate the production of antibodies in addition to photoactivation of TGF β1 that are specific to the UV-exposed infectious agent. The central checkpoint role of the TGF-β pathway in embryonic development, immune responses, tissue healing, and malignancies is now well established. Among various biophysical wound management approaches, low dose biophotonics treatments (Photobiomodulation or PBM), has also gained favorable attention. The PBM molecular mechanism of PBM treatments includes photoactivation of latent TGF β1 response, which. contributes a key role in promoting wound healing and tissue regeneration. Additionally, the irradiation-denatured protein entities may also stimulate antigenic-specific humeral neutralizing antibody responses which may result in the formation of immunoglobulin classes IgG, IgM,and others over the course of days or weeks following the UV exposure [8]. The PBM treatments are not known to result in untoward effects [26-33]. Thelow levelbiostimulation process promotes cell survival and proliferation both in vitro and in vivo and supports an action to mediate increases in the generation of “good” Reactive Oxygen (ROS) species that can activate redox sensitive signal transduction pathways including Nrf-2, NF-kB, and ERK. These responses act collectively at key redox checkpoints in the cell cycle to enabling cell survival and replication mechanisms and in proliferation and survival of affected tissues. Also, the bio-stimulation process improves oxygen delivery to peripheral tissues via laser-induced photodissociation of oxygen from oxyhemoglobin in cutaneous blood. The increases in blood SpO2 saturation further contribute to the role of biophotonics in the regenerative processes that contribute to tissue regeneration and healing [33-35]. Additionally, the percentages of hemoglobin A1c decreased with the increases in blood SpO2 following multiple cycles of biophotonic therapy [36].
Inactivation of viruses and microorganisms may occur in encapsulated viruses following chemical disruption of infectious agent proteins and other constituents. In SARS-CoV-2, the coronal spike proteins are responsible for the initial Angiotensin-Converting Enzyme 2 (ACE2) receptor membrane fusion event, facilitated by lipid-lipid interactions between the coronal and the plasma membrane lipids. The spike protein-ACE2 interaction allows the virus to quickly enter the host cell and cause infection [8,9]. The outermost corona of Coronaviridiae consists of a protective lipoprotein-rich bilayer shell, thereby providing the virus limited protective influences that enhance its survival when contained in both in vivo and in vitro environments including aerosol microdroplet migration. Once bound to the receptor, the coronal lipid can then facilitate viral entry into lipid rich plasma membranes and enables further access to cytoplasmic constituents needed to undergo intracellular host viral replication. The complimentary immunochemical events during spike protein attachment facilitate an efficient viral association with receptive ACE2 receptors of respiratory, neural, intestinal, and other tissues [36-38]. Chemical agents including short chain alcohols are miscible with the coronal lipid composition and can readily disrupt and dissolve the coronal lipid and disrupt immunoreceptor binding. Chlorine bleaches and other disinfectants can also cause disruption and disinfection of both exposed mammalian and inanimate surfaces including skin, mucosal membranes, countertops, handrails, and other items following aerosol-mediated microdroplet distribution [38].
Because of the aerosol microdroplet infectious potential of airborne particles may be carried for considerable distances by prevailing airflow, diluted only by the surrounding airspace, containment is difficult [8,9]. Because an infective dose of most organisms may travel at least ~6 feet (~2 meters) from its origin, the contaminated airspace poses an invisible infectious risk for many individuals, particularly for those individuals with a compromised immune system [29]. Similar chemical disinfection actions also result for most encapsulated and unencapsulated microbial agents, and when chemical disinfectants are combined with controlled irradiation, the combination can effectively decontaminate microbial and viral agents in both impacted airspaces, surfaces and inanimate objects [9,38].
Objectives, method, and summary of research
The objectives of this brief communication were to provide a brief history of epidemics and pandemics, the biological mechanisms of biophotonic therapy, and to summarize the overall reported effectiveness of the Einstein Adjuvant Energy Dynamics/Einstein Matrix methods in applying biophotonics to the treatment and amelioration of infectious illnesses, where the biophotonics treatments were deemed the primary key elements in the treatment and symptomatic amelioration of refractory viral and microbial infectious illnesses. The studies reviewed were conducted in approved clinical research setting in the Einstein Medical Clinic in Dominican Republic. The complexity of the pre-existing physical and physiological biological variables reported became evident among most patient histories and symptoms. The Einstein Adjuvant Energy Dynamics/Einstein Matrix method of the present review included [9,38,39]:
- Psycho-Video diagnostic assessment followed by and in concert with Psycho video therapy;
- Biophotonics irradiation therapy via standardized protocols, and
- Electromagnetic alternating current dynamic therapy
The biophotonics procedure employed involved aseptically removing 100 to 200 ml of the patient’s blood in a sterile heparinized vessel, followed by gentle mixing it with 200 to 400 ml of intravenous grade neutral saline. The blood-saline dilution was then passed through a sterile quartz UV irradiation chamber exposed to both UVA and UVC. The blood dilution was reinfused over an approximate 30-minute time frame as previously described [28,29]. The procedures were always conducted under strict medical supervision in an out-patient clinical setting. In the co-author’s experience with hundreds of patient events, no negative side effects were reported. The effective coherence of sigma quanta energy dynamics is consistent with the theory of Einstein Human Bioenergetics and Natural Homeostasis Systems of Biophysical and Biochemical Therapy. This approach was applied to treatment of viral, bacterial and fungal infections in the Einstein clinic [25-27].
To apply biophotonics and electromagnetism to defeat coronavirus infections, the physical methods summarized could avoid the often-unpredictable pitfalls of chemical-based therapeutic approaches [28,29]. The specific biophotonics and electromagnetism therapy was applied for the therapy of HIV/Aids, Hepatitis C and to Methicillin-Resistant Staphylococcus Aureus (MRSA) infections. The patients received the entirety of their treatments at the Einstein Clinical Laboratories Case Studies Research Laboratories in the Dominican Republic during the years 2001-2003, where over 100 patients were studied [4,29,30,40,41]. The specific wavelengths and dosages applied remain privileged, proprietary information of the Einstein Medical Institute at this time.
During the cited research, a highly elevated level of success was attained [40,41,42-49]. Moreover, no incidents, reports, or observation of occurrence of adverse effects of any sort were observed or reported after conducting the therapeutic evaluations. Treatment sessions were followed up by 4 weeks of additional repeated biophotonic and electromagnetic treatment, administered twice-weekly within a one-month timeframe, each receiving an average of 10 treatment sessions [28,29,39,40]. Patients remained asymptomatic with improved health thereafter. The studies conducted adhered to the criterion of the Helsinki guidelines, were approved by the USAT and EMI Institutional Review Boards and were in compliance with the local governmental and Ministry of Health agreements.
The summary of results of biophotonic treatments were highly favorable with no recurrence reported. The video combined Einstein method has the potential to make an early assessment of patients regardless of their level of advancement and instability of their illness. Careful assessment and monitoring can better estimate the magnitude and duration of treatments deemed necessary to resolve their illnesses [40,41]. The proposed Einstein approach may effectively address the possible concurrent emotional and intuitive elements of SARS-2-COVID-19 and other infectious illnesses, and comorbidities of other aspects of infectious illnesses when present [50]. This multifaceted approach enabled the investigators to develop individualized strategies that were observed to improve their overall health and mental well-being during and after recovery of the patient. The effective applications of electromagnetic potential therapies added to the proposed biophotonic therapy for infectious diseases are currently presumed experimental and require additional research and evaluation via both in vitro and in vivo methodologies. The multifaceted approach was utilized while conducting the earlier case studies on HIV/AIDS, Hepatitis C and methicillin resistant Staphylococcus aureus in the Dominican Republic Einstein clinic over a three year duration of observation (2001-2003) in the cited clinic [19-23,25, 26,39,40,48,49]. Circulating inflammatory cytokine levels including IL-6 and others were observed to become consistently decreased following the biophotonic treatments, and immunologic parameters also demonstrated measurable physiologic and clinical improvement as patients recovered from the viral and microbial infections [26,27,48,49].
Discussion
According to Einstein Medical Institute case studies, the research results demonstrated that the combined impact of bioelectromagnetic and biophotonic therapeutic treatments for RNA-viral and antibiotic resistant Staphylococcus aureus infection therapy were deemed effective therapies. Favorable results included decreasing the viral and bacterial loads, decreasing the generation of inflammatory cytokines, and diminishing the magnitude of the pathophysiologic sequela of the infections [10,26,27,41,42]. In addition, because the biophotonic and biomagnetic treatments resulted in enhancement of immunologic parameters, this suggests that this therapeutic approach may be an efficient, timely and cost-effective clinical option to treat the complexity of COVID-19 and other infections [42]. This therapeutic approach may reduce both the magnitude and duration of acute infections and their consequential longer-term sequela during both active and convalescent periods of microbial and viral infection. These benefits are also predicted to include the chronic symptomology of long-covid and antimicrobial resistant microbial infections. As with prescribing a treatment regimen for any infectious disease, early intervention is always highly preferable. Moreover, because of the absence of antimicrobial or antiviral resistance the treatments to biophotonics, the regimen remained effective.
Early resolution of such infectious illnesses is likely to result in not only a more complete recovery but also a decreased magnitude of comorbidity of exacerbations secondary to the presenting infectious illness under study [8]. In as much as biophotonic and bioelectromagnetic therapy is not substantially reliant on allopathic drugs or chemical medications, it emerges as a most cost-effective approach to manage and treat emerging infectious illnesses globally. In addition, this may be accomplished without the overwhelming financial impact on institutional resources. Moreover, as aside from the initial cost of the UV apparatus, the costs of disposable IV apparatus and supporting expendable supplies to conduct the treatments is relatively minimal in comparison to current therapeutic protocols [41,42,49].
The detailed molecular or biochemical mechanisms of action through which therapeutic biophotonic and magnetic exposure may ameliorate the infectious load and magnitude of infections remains speculative. To date, in vitro studies confirmed the development of deleterious genomic cell-cycle effects on infectious viral agents and microorganisms studied following irradiation to date which prevent their further replication in the host. This blockade effectively likely prevents further in vitro, and host-supported in vivo replication of the infectious agents. Ultraviolent light is known to be viricidal and microcidal and to exhibit the capacity to impact disabling structural damage to RNA, DNA, and nuclear polymers, thereby likely impairing their viability and continued regeneration [28-32]. In a recent studies, biophotonic therapy was also found to improve hemoglobin oxygen saturation as indicated by increases in blood SpO2 within minutes after the onset of the biophotonic treatment [38]. Levels of hemoglobin A1c were also decreased by a similar proportion to the improvements in SpO2 with only a few treatments [38]. Typically complete symptom resolution occurred within 72 hours, thereby likely impacting on an improved redox potential of the perfused tissues [34-36].
The comorbidities of obesity, along with NIDDM, hypertension, respiratory disease, disordered bioenergetics, and other pathophysiologic complicating processes are significant risk factors in the progression of complications in COVID-19 illness. The comorbidities are significant in both vaccinated and unvaccinated individuals [9,24,26]. The coronavirus causing COVID-19, SARS-CoV-2 has some similarities to the emergence of earlier reports of other zoonotic coronavirus illnesses including MERS and SARS which also caused respiratory illness in humans [5-7]. The origin of SARS-COV-2 remains unclear, but appears to have originated in a Wuhan, China environment in late 2019 as a local epidemic. Within a few months the virus had spread throughout the globe and was declared a pandemic by the WHO within three months of its first report to the WHO [6,41].
The corona virus enters mammalian organ systems via widely distributed ACE2 receptors many receptive tissues and organs. After infection it can produce a myriad of symptoms easily associated with non-viral origins and which may confuse an initial diagnosis [9,10]. Thus, the virus can interact via the infective spike protein domains in multiple organs and tissues throughout the body that have ACE2 receptors, including the respiratory epithelium where it has received the most notoriety. Once visceral adipose tissue becomes infected, it initiates the release of inflammatory cytokines including IL-6, TNF, and others. The inflammatory cytokines can quickly lead to a serious and an often-fatal cytokine storm [10,25]. Since human obesity develops via hyperplasia and hypertrophy of preadipocytes, the adipocytes once differentiated likely retain their genetically determined cell surface receptor domains and intracellular biosynthetic functions thereafter. The increased adipose mass thus formed, especially when combined increasing BMI of >30 is associated with glucose intolerance and NIDDM. The increased visceral adipose tissue mass and additional comorbidities appears to reflect a proportionately greater risk of cytokine mediated complications from COVID-19 [9,10,24]. Similar ACE2 receptor domains occur on the receptive surfaces of tissues of other organs.
Once receptive tissues become infected with the virus, the intracellular viral replication occurs rapidly and may spread to other receptive tissues, while normal immune responses tend to lag behind the viral replicative events in both unvaccinated and many vaccinated individuals [9,10,12]. In severe cases, death may occur due to a combination of the additive impact of the virus and comorbidities. Additionally, the more advanced the individual or multiple comorbidities, the more severe magnitude of illness may occur [9,22]. Restoration of a healthy BMI in obesity and overweight conditions is typically a gradual and often unrewarding process, as the improvements in BMI are often only temporary in duration as weight regain occurs easily when therapeutic regimens are relaxed or discontinued. Weight loss toward a normalization of BMI and an otherwise healthy weight is associated with smaller adipocyte size and corresponding adipocyte surface area and can decrease the relative risks for other comorbidities over time. However, the magnitude of risk reduction for COVID-19 following weight loss remains unclear. In non-adipose tissues, the ACE2 receptors remain present and active, likely facilitating reinfection by older and mutated epitopes of the spike proteins only months following active infection or immunization [10,40,41].
Conclusions
In conclusion, NIDDM, respiratory illness and overweight and obese conditions that increase visceral fat deposition and ACE2 receptor site distribution may progressively increase the relative risk for the most severe complications of the COVID-19 illness. Early intervention via biophotonic and bioelectromagnetic therapies may provide a useful and cost-effective adjunct in the treatment and prevention of infectious illness. Thus, biophotonics may be especially useful for those infections where pharmaceutic or chemical agents may have become ineffective. Moreover, the coherence of biophotonic/electromagnetic immuno-stimulation therapy measures via potentiation of adjuvant energy dynamics in SARS, MERS, COVID-19, and other viral and microbial infections may become a useful strategy. When applied, it may decrease the magnitude of pathophysiologic sequala that typically follow the infectious process. Future studies are recommended to further evaluate and quantify the clinical benefits that may be obtained by applying biophotonic and bioelectronic therapies. Future studies may successfully determine the minimally and maximally effective ranges of dosages of biophotonic and biomagnetic applications required to treat such illnesses in the most effective, efficacious, and beneficial manner.
The many previously undefined therapeutic benefits of sunlight exposure have been practiced in cultures for thousands of years, long before the discovery of the photon. The introduction of countless newly-discovered molecular biological approaches in the treatment of human illness and disease, and when combined with the contributions of modern therapeutic approaches the benefits are likely to continue well into the next millennia. Biophotonic therapies have been found to be well tolerated in clinical use and human tissues have been observed to tolerate the procedure without incident in recent studies. Controlled clinical exposure of human tissues in addition to inanimate surroundings to broad ranges of UV irradiation spectra can effectively injure microbial and viral genomes and denature their proteins both in vivo and in vitro. The UV-mediated injuries occur regardless of their sensitivity or resistance to conventional antimicrobial or antiviral agents. Thus, impairing the capacity of invasive infectious agents for continued host-supported parasitic replication at the metabolic and nutritive expense of their benefactor is a viable strategy in their treatment. In addition, enhancing host immune response mechanisms without injurious effects on human tissues can enable patients with the most severe and often seemingly intractable infectious illnesses to undergo an uneventful and likely complete recovery.
Acknowledgments
The authors are grateful for the many supportive patients who have voluntarily undergone biophotonic and biomagnetic treatments, and the numerous graduate students and colleagues who have contributed to these studies. The authors also acknowledge the Institutional support of the University of Science Arts and Technology and the Einstein Medical Institute provided to complete the above manuscript.
References
- Sakai T, Morimoto Y. The history of infectious diseases and medicine. Pathogens 2022;11(10):1147.
[Crossref] [Google Scholar] [PubMed]
- Reygaert WC. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS microbial 2018;4(3):482.
[Crossref] [Google Scholar] [PubMed]
- Goda K. Biophotonics and beyond. APL Photonics 2019;4(5):1-3.
- Einstein GP, Tulp OL, Anaushvili A. Comparative effects of biophotonic therapies in viral and microbial illness. Biom Biostat Int J 2023;12(1):23-25.
[Crossref]
- International committee on taxonomy of viruses.UK: International Committee on Taxonomy of Viruses (ICTV) 2019.
- Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 2019;17(3):181-192.
[Crossref] [Google Scholar] [PubMed]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382(8):727-733.
[Google Scholar] [PubMed]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020;395(10223):507-513.
[Crossref] [Google Scholar] [PubMed]
- Schroeder S, Mache C, Kleine-Weber H, Corman VM, Muth D, Richter A, et al. Functional comparison of MERS-coronavirus lineages reveals increased replicative fitness of the recombinant lineage 5. Nat Commun 2021;12(1):5324.
[Crossref] [Google Scholar] [PubMed]
- Tulp OL, Awan AR, Einstein GP. SARS-CoV-2: Respiratory and gastrointestinal pathobiology of the corona virus illness, COVID-19. Gastroenterol Hepatol 2021;12(3):82-87.
- Noh JY, Jeong HW, Shin EC. SARS-CoV-2 mutations, vaccines, and immunity: Implication of variants of concern. Signal Transduct Target Ther. 2021;6(1):203.
[Crossref] [Google Scholar] [PubMed]
- Omicron variant: What you need to know. CDC Centers for Disease Prevention and Control 2021.
- Elflein J. Coronavirus (COVID-19) in the USA-Statistics and Facts. Health, Pharma & Medtech 2023.
- Capasso A. Biomedical applications of biophotonics. J Biochem Biotech 2021;4(1):6.
- Rizvi SA, Einstein GP, Tulp OL, Sainvil F, Branly R. Introduction to traditional medicine and their role in prevention and treatment of emerging and re-emerging diseases. Biomolecules 2022;12(10):1442.
[Crossref] [Google Scholar] [PubMed]
- Rizvi SA, Einstein GP, Tulp OL, Sainvil F, Branly R. Applications of traditional medicines in prevention and treatment of the diseases of humankind. Pharm Sci 2023;9:1-50.
- Spyrou MA, Tukhbatova RI, Wang CC, Valtueña AA, Lankapalli AK, Kondrashin VV, et al. Analysis of 3800-year-old Yersinia pestis genomes suggests bronze age origin for bubonic plague. Nat Commun 2018;9(1):2234.
[Crossref] [Google Scholar] [PubMed]
- Sanon V, Sainvil F, Awan AR, Einstein GP, Tulp OL. Haiti’s cholera epidemic: Will it return in 2021. Gastroenterol Hepatol 2021;12(4):124-126.
- Murray PF, Rosenthal KS, Pfaller M. Medical microbiology, 8th Edition. Elsevier 2021.
- Finkelstein RA. Cholera, Vibrio cholerae O1 and O139, and other pathogenic vibrios. Medical Microbiology. 4th edition. 1996.
[Google Scholar] [PubMed]
- Highly Pathogenic Avian Influenza A (H5N1) in birds and other animals. CDC 2020.
- H5N1 genetic changes inventory: A tool for international surveillance. CDC 2020.
- Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty 2020;9(02):23-29.
[Crossref] [Google Scholar] [PubMed]
- Kim SY, Yoo DM, Min C, Wee JH, Kim JH, Choi HG. Analysis of mortality and morbidity in COVID-19 patients with obesity using clinical epidemiological data from the Korean center for disease control and prevention. Int J Environ Res Public Health 2020;17(24):9336.
[Crossref] [Google Scholar] [PubMed]
- Sanoudou D, Hill MA, Belanger MJ, Arao K, Mantzoros CS. Obesity, metabolic phenotypes and COVID-19. Metabolism 2022;128:155121.
[Crossref] [Google Scholar] [PubMed]
- Tulp OL, Einstein GP. The evolution and global impact of COVID-19 and Omicron: The way forward. Int J Family and Comm Med 2022;6(1):11-13.
[Crossref]
- Tulp OL, Einstein GP. Obesity and its associated inflammatory cytokines pose significant risk factors for COVID–19 outcomes. Adv Obes Weight Manag Control 2022;12(1):14-20.
- Tulp O, Sciranka A, Sainvil F, Einstein GP. The role of adiposity, body mass index, aging, and chronic comorbidities on progression of COVID-19 illness. Is a long COVID syndrome inevitable? Int J of Family and Commun Med 2022;6(3):99-104.
[Crossref]
- Einstein G, Echavarria L, Tulp O. Application of Einstein matrix medical treatment for HIVv/HCV therapy (668.4). Faseb J 2014;28:668.4.
- Einstein GP, Kowalczewska M, Tulp OL. Biophotonic and bioenergetic phototherapy for treatment of Antimicrobial Resistant S Aureus Infection (ARSI). Faseb J 2012;26(S1):733
- Peng W, Shaw BR. Accelerated deamination of cytosine residues in UV-induced cyclobutane pyrimidine dimers leads to CC→ TT transitions. Biochemistry 1996;35(31):10172-10181.
[Crossref] [Google Scholar] [PubMed]
- Hume AJ, Ames J, Rennick LJ, Duprex WP, Marzi A, Tonkiss J, et al. Inactivation of RNA viruses by gamma irradiation: A study on mitigating factors. Viruses 2016;8(7):204.
[Crossref] [Google Scholar] [PubMed]
- Oguma K, Kanazawa K, Kasuga I, Takizawa S. Effects of UV irradiation by light emitting diodes on heterotrophic bacteria in tap water. Photochem Photobiol 2018;94(3):570-576.
[Crossref] [Google Scholar] [PubMed]
- Sadraeian M, Zhang L, Aavani F, Biazar E, Jin D. Viral inactivation by light. eLight. 2022;2(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Krasnovsky AA, Drozdova NN, Roumbal YV, Ivanov AV, Ambartzumian RV. Biophotonics of molecular oxygen: activation efficiencies upon direct and photosensitized excitation. Chin Opt Lett 2005;3(101):S1-S4.
- Asimov MM. Biophotonics of new optical method of regulating oxygen concentration in biological tissue. 11th International Conf 2011:1-3.
- Masaud SM, Szasz O, Szasz AM, Ejaz H, Anwar RA, Szasz A. A potential bioelectromagnetic method to slow down the progression and prevent the development of ultimate pulmonary fibrosis by COVID-19. Front Immunol 2020;11:3199.
[Crossref] [Google Scholar] [PubMed]
- Bently RE. The mechanism of increased tissue oxygenation via bio-photonic therapy. 2015: 110.
- DiRuzzo J, Kerna N, Di Ruzzo J. Coronavirus now: A timely and practical summary of the current epidemiological information, clinical presentation and prevention and treatment of 2019-nCoV (2019 novel coronavirus). EC Emerg Med and Crit Care 2020;4(4):25-31.
- Bassey GO, Einstein GP, Tulp OL. Contemporary treatment of antimicrobial resistant S. aureus, HCV and HIV infection: A case study. Faseb J 2020;34(S1):1.
- Einstein GP, Tulp OL. Integrated sigma dynamics quantum energy therapy presented by mathematical function and matrices in immunologic stimulation. Faseb J 2017;31(S1):lb805.
- West BJ. Where medicine went wrong: Rediscovering the path to complexity. World Scientific 2006;11:352.
- WHO report of WHO announcements regarding SARS-CoV-2. 2022.
- Joint WH. WHO-convened global study of origins of SARS-CoV-2: China part. 2021.
- Rahman SU, Mosca RC, Govindool Reddy S, Nunez SC, Andreana S, Mang TS, et al. Learning from clinical phenotypes: Low‐dose biophotonics therapies in oral diseases. Oral Dis 2018;24(1-2):261-276.
[Crossref] [Google Scholar] [PubMed]
- Nogueira MS. Ultraviolet-based biophotonic technologies for control and prevention of COVID-19, SARS and related disorders. Photodiagnosis Photodyn Ther 2020;31:101890.
[Crossref] [Google Scholar] [PubMed]
- Stasko N, Kocher JF, Annas A, Henson I, Seitz TS, Miller JM, et al. Visible blue light inhibits infection and replication of SARS-CoV-2 at doses that are well-tolerated by human respiratory tissue. Sci Rep 2021;11(1):20595.
[Crossref] [Google Scholar] [PubMed]
- Einstein GP, Tulp OL, Anaushvili A. Coherence of sigma quanta electromagnetic immune-stimulation via potentiation of adjuvant energy dynamics in SARS-2-COVID-19: An RNA virus case study. FASEB J 2022;36(S1).
- Einstein GP, Tulp OL. The recent origin, evolution, and containment of RNA viruses: MERS, SARS, and COVID-19 and their impact on global healthcare: An editorial perspective. J Health Econ Outcome Res 2022;8(1): 001-007.